D3G's 'MH LIFECOURSE CONCEPT' AND 'D3-CHALKY TEETH LINGO'
D3G has reconceptualised the topic of molar hypomineralisation ("MH") and chalky teeth to fit the modern ideals of science translation and preventive healthcare. Building on strengths of the DDE and MIH eras, our new 'MH lifecourse concept' embodies scientific rigour, medical prevention, and translation to social good. This revolutionary concept and its partnered language ("translational lingo") together comprise a valuable paradigm shift for the field, as acknowledged by a leading academic journal in 2024.
Looking back at 2010, it was clear to D3G researchers that prevailing terminology for the broader problem we today call MH was scientifically inadequate. Key limitations of the popular clinical term "Molar Incisor Hypomineralisation ("MIH") were under-representation of the problem scope, and disharmony with D3G's goal of prevention. Over the following decade, D3G took a translational approach to:
(1) Develop a stronger definition for MH that emphasises scientific hallmarks and eliminates widespread confusion surrounding incisors;
(2) Introduce an underpinning classification for MH and other "demarcated opacity disorders" ("DODs") based on learnings from the scientifically-strong DDE era; and
(3) Adopt a lifecourse approach, recognising MH involves both the baby and adult teeth and so is best attacked progressively from the beginning.
(4) Craft a "translational lingo" (special language, or terminology)
that enables conversation progressing from either public-friendly
("chalky teeth") or scientifically-precise starting points.
The following definition, classification and lifecourse approach to MH – which together comprise D3G's 'lifecourse concept of MH' - remain academic works in progress. This new translational concept, and its interlinked 'D3-chalky teeth lingo' (here, here), are expected to evolve both as our scientific understanding grows and the needs of diverse audiences are increasingly accommodated.
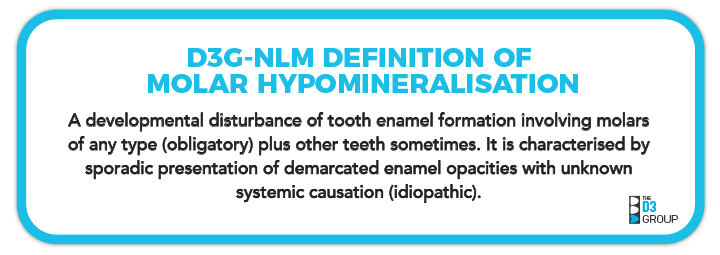
D3G-NLM DEFINITION OF MOLAR HYPOMINERALISATION

In 2023, the US National Library of Medicine (NLM, host of MEDLINE & PubMed) published a concise academic definition of Molar Hypomineralisation (MH), in association with D3G. The wording was designed to cross-reference two related bibliographic subject headings (amelogenesis, molars). NLM's dental MeSH tree was also collaboratively revised to correct misclassification of dental enamel hypoplasia and embrace clinico-scientific foundations established by Grace Suckling and contemporaries during the DDE era (D3G+NLM, manuscript in preparation). D3G added translational value to NLM's definition by emphasising both sporadic presentation and unknown systemic causation (idiopathic) as scientific hallmarks of MH, and describing the enamel-formation process more simply.
Our ensuing concise academic definition of MH is:
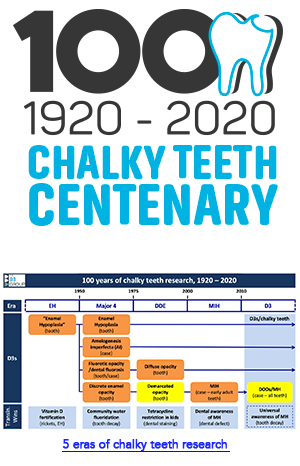
This field-reshaping advance followed widespread consultation and peer review, both across the sector and around the world (Toronto International D3 Symposia, 2020-2022), together with publication of a historical review of "chalky teeth research". This consensus-seeking process also prompted development of an MH Green Paper, that supports not only the above concise academic definition, but also provides three other definitions of MH optimised for specialist, professional and public audiences (see below).
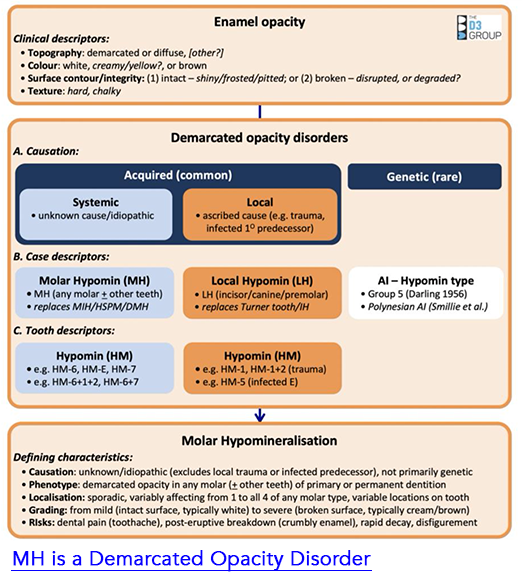
DRAFT CLASSIFICATION OF MH AS A 'DEMARCATED OPACITY DISORDER'
Surprisingly, a published classification was lacking for MH, perhaps reflecting the common misconception it is a "new condition". To provide clinical and scientific context for our definition of MH, D3G has drafted a classification scheme for MH and other conditions involving dental enamel opacities that appear solidly distinct from normal enamel (i.e. "demarcated", as opposed to "diffuse") – we collectively term these "demarcated opacity disorders" or "DODs" for short.
Having been "discovered" late in the first century of chalky enamel research, MH needs to be considered in view of what came earlier, particularly during the DDE era. Such clinical and scientific appraisals indicate MH is a distinct type of DOD. Classification of MH therefore necessitates formulation of a broader scheme embracing other known DODs and enamel opacities in general. As portrayed in our draft DOD Classification infographic (right, published here), once demarcated opacities are defined as a subgroup of enamel opacities, attention turns to their primary causation (acquired or genetic). Acquired DODs are then categorised at case level as having systemic origins (e.g. MH), as distinct from local causation. MH cases can then be characterised at hypomineralised (HM) tooth level by combining two popular dental notations to distinguish baby and adult dentitions.
Beneficially in both the clinic and lab, this strategy provides a translationally-robust, diagnostic flow from demarcated opacity to "HM tooth" to "MH kid". Further details appear in our MH Green Paper (see below).
A LIFECOURSE APPROACH TO MH
By embracing the whole dentition – from earliest baby teeth through to wisdom teeth in early adulthood – D3G's scientific approach to "MH" enjoys all the medical and social benefits of modern lifecourse theory. This "timeline approach" follows an individual's life history from the beginning and considers multiple influences (e.g. medical, environmental, socioeconomic) during development from a baby into adulthood. Strong alignments can then be made with the medical origins of MH, maternal and child health and allied inequality issues. Importantly, this lifecourse platform also highlights MH as a potentially preventable birth defect – as explained to families in 'Sam's Story'.
Our switch to 'MH lifecourse' thinking has necessitated a major revision of terminology and clinical reporting. Hence, we refer to back teeth at most risk of being chalky in order of their eruption into the mouth – starting with 2-year molars, then 6-year and 12-year molars, and finally the wisdom teeth (18-year molars). Our unique compilation of MH prevalence studies exemplifies this new approach, and ensuing benefits for MH prevention at dental and medical levels are noted below.
D3G'S ACADEMIC CASE & LEAD ADOPTERS OF OUR 'MH LIFECOURSE CONCEPT'
D3G's academic case for evolving D3 terminology and introducing our lifecourse concept of MH involved three
main initiatives:
(1) Resolving chaos of the MIH era (see below);
(2) Better referencing of the scientifically-strong DDE era; and
(3) Establishing a lifecourse platform for MH.
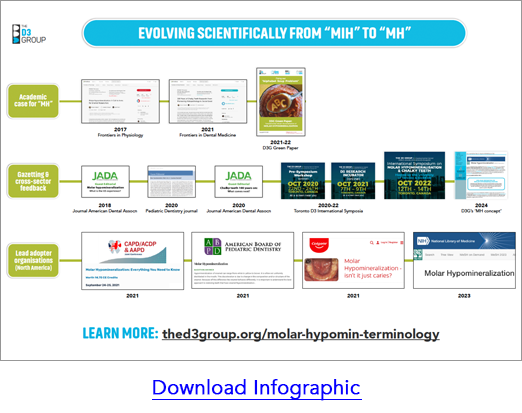
Publicising this work commenced with the 2017 publication of
a call to arms article about MH that targetted scientifically-inclined readers. Such emphasis on a cohesive whole-dentition mindset was shared with clinical audiences via
guest editorials in widely-read dental journals (JADA 2018, Pediatric Dentistry 2020, JADA 2020). Translational exposure
to interested parties from across the sector and around the world was achieved via our Toronto D3 Symposia (2020, 2021, 2022) and accompanying MH Green Paper (see below). During this time, North American paediatric dentistry organisations (AAPD, CAPD, ABPD), and an educationally-active multinational company (Colgate), embraced the term "MH" independently in far-reaching educational settings, as illustrated in this infographic. The term "MH" also starred in a top-ranking scientific journal (Proceedings of the National Academy of Science, USA) in 2022. Adding wonderful icing to this D3 cake, USA's authoritative NLM did a long-needed "D3 makeover" at bibliographic-database level, including the concise academic definition of MH above. This was followed in 2024 with the first adoption by an academic journal of D3G's translational paradigm (Pediatric Dentistry editorial), marking a major milestone for the MH Lifecourse concept.
WHAT BENEFITS DOES "MH" HAVE OVER "MIH ALPHABET SOUP"?
As elaborated here, the MIH era benefitted our field by increasing awareness around MH, particularly in clinical dentistry contexts. Unfortunately, those two "MIH decades" became plagued by terminological chaos – which we nickname "the alphabet soup problem" (see below). In contrast to this fragmented era of "MIH alphabet soup", the holistic thinking behind our D3G-NLM definition of MH has three core benefits, each aligning with D3G's science to social good mission.
1. STRONGER SCIENCE

Full scope of the problem:
As a case descriptor, "MH" addresses the whole problem of idiopathic demarcated opacities, as they present across both dentitions (i.e. baby and adult teeth). Conversely, "MIH" involves early-erupting adult teeth only, and so risks "tunnel vision" – both scientifically and clinically. Consequent reliance on other terms for baby and later-erupting adult teeth also gives false impression of distinct conditions (e.g. MIH, HSPM, HOPT; see below) – rather than the reality of MH being a medico-dental "spectrum disorder".
Understanding causation:
Critically for investigation of medical causation (aetiology), "MH" avoids the diagnostic uncertainties associated with chalky adult incisors. In contrast, "MIH" is aetiologically compromised by uncertainties whether demarcated opacities on adult incisors have local origins (so-called "Turner teeth") or systemic origins – technically, this uncertainty is called aetiological confounding. Focussing instead on molars at case level provides an "aetiologically clean" way to study the medical origins (i.e. idiopathic, systemic causation) and prevention of MH. What then happens to hypomineralised adult incisors, which remain problematic for clinicians and affected kids alike? Generally, it's best to "drop" from case- to tooth level and simply call them "hypomin incisors" (HM-incisors) – this avoids the causation issue. However, when HM-incisors seemingly do have idiopathic systemic causation, then they (and any other teeth with idiopathic demarcated opacities) are scientifically included in an "MH" case (read more).
2. BETTER PREVENTIVE PRACTICE
'MH lifecourse' approach:
As above, by including all teeth in the baby and adult dentitions, D3G's 'MH lifecourse' approach aligns with the medical, environmental and socioeconomic considerations of modern lifecourse theory. The holistic nature of ensuing understanding (the "gestalt of MH") will benefit both clinical and public-health practice. From a prevention standpoint, this approach provides a logical order of attack and makes for easy communication about the invisible delay between a child's age at medical onset of chalky enamel (i.e. when hypomineralisation happened inside the jaw) and later "dental ages" when chalky teeth erupt into the mouth (2-year, 6-year, 12-year & 18-year molars). Conversely, "MIH" addresses just the middle part of this dental spectrum (6-year molars), leading to the "alphabet soup" of terms describing other stages and manifestions.
Dental prevention:
Targetting preventive healthcare at population level, D3G's 'MH lifecourse' approach encourages "chalky teeth screening" from early ages (e.g. 18+ months for chalky baby canines, 24+ months for chalky 2-year molars). Such early detection maximises not only opportunities for dental professionals to act preventively, but also enables affected families and their dental advisors to anticipate chalky teeth erupting at later ages. As a result of this preventive strategy, identified "chalky teeth kids" may have substantially lower need for complicated (expensive) dentistry. Conversely, "MIH" is unhelpful in this regard, being focussed on adult teeth only.
Medical prevention:
If we're to learn how to prevent MH medically – that is, by stopping chalky enamel (hypomineralisation) from happening in the first place – we must understand its causation across the full range of medical-onset ages. The origin of MH spans from birth (baby teeth) through to adolescence (wisdom teeth). Our "MH lifecourse" approach supports this quest, whereas "MIH" again risks "tunnel vision" aetiologically.
3. SOCIAL GOOD
'D3 science to social good':
Together, MH affecting 1 in 5 kids worldwide, plus its associated burden of tooth decay and dental pain, underpins massive social damage across our planet. A correspondingly huge opportunity to benefit global society seems likely once a medical-prevention strategy is identified and successfully implemented. To achieve this exciting goal, we need strong science and an 'MH lifecourse' approach as noted above. From first principles at least, we can surely expect that "translational MH thinking" will get us there much faster than "MIH tunnel vision" and all its chaotic baggage.
'Good for D3 science':
A reciprocal benefit of stronger D3 science being good for society is that social awareness of the chalky teeth/MH problem should benefit scientific endeavours to prevent it.
"ALPHABET-SOUP PROBLEM" AND OUR "MH GREEN PAPER" SOLUTION
Urgent need for a translationally robust characterisation of MH became a catch-cry of the 2020 D3 Workshop – our inaugural international-consensus-seeking event for "Molar Hypomin and Chalky Teeth". Particular concerns revolved around the chaotic – and scientifically untenable – set of terms that had been published over the preceeding 20 years (i.e. MIH era). Drawing on the alphabet soup metaphor, we nicknamed this "the Alphabet Soup Problem".
The MIH era's "Alphabet Soup Problem"
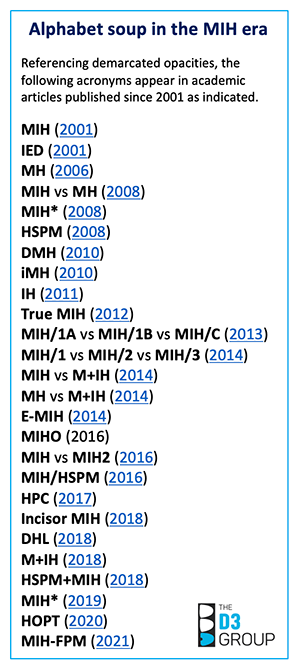
Scientifically at least, it's disturbing that the academic literature has accumulated at least 25 other terms referencing “demarcated opacities” since the term “MIH” (molar-incisor hypomineralisation) was introduced in 2001. The most-prevalent accessory terms include "HSPM", "DMH" and "IH" – standing for hypomineralised second primary molars (same thing as 2-year molars), deciduous molar hypomineralisation and incisor hypomineralisation, respectively. Yet key gaps remain despite this confusing "MIH alphabet soup". A notable absence is hypomineralised 12-year molars which comprise a second type of "HSPM" (hypomineralised second permanent molars) by above convention – talk about confusing! Is this shemozzle of terms and acronyms good for science, clinical practice and communication? Clearly not – but what to do about it and how?
D3G's Green Paper on "Fixing our Alphabet Soup Problem"
Unsurprisingly given our translational mission, D3G invited all main stakeholders (researchers, reviewers, publishers, funders, educators, industry, affected public) to team up and fix this "alphabet soup problem” together. Drawing on a decade of listening, learning and testing the waters, we drafted a Green Paper initially titled 'Fixing our Alphabet Soup Problem'. It outlined a translational characterisation of MH that's scientifically robust and historically accurate. Following international, multi-stakeholder critique at the 2021 D3 Research Incubator, a revised draft – titled 'Translationally Robust Characterisation of Molar Hypomineralisation as a Demarcated Opacity Disorder' – was given a second “translational peer review” at the 2022 International D3 Symposium in Toronto, leading to further revision.
With a working consensus achieved at "D3 aficionado" level, D3G is now striving to ensure broader workability of our
"MH-DOD concept" across the sector and around the globe.
For starters, the latest iteration was provided to a broad audience of interested dental researchers (D3 Day at IADR) and various other stakeholder groups will be approached for their critique next. Meanwhile, interested individuals can access the 'MH Green Paper' through our D3 Learning Loop.
LEARN MORE AND SHARE YOUR THOUGHTS
Read more in our Writer & Reviewer Guide about how "hypomin terminology" – being "Hypomin enamel" (HM-enamel or HM-spots or HM-teeth) at tooth level and "Molar Hypomin" (MH) at case level – integrates with other basic and specialist "lingo" (aka "translational term-sets").
As always at D3G, your feedback and enquiries are welcomed (contact us).