The Basics
TOWARDS A TRANSLATIONAL SET OF D3 TERMS ("D3-CHALKY TEETH LINGO")
As noted here, D3G aims to develop guidelines that are both clinically useful and research friendly – and of course robust terminology lies at the heart of this aim. For over a decade, we've obtained collaborative input from key stakeholder communities (scientists, dental & medical practitioners, industry, public), leading to the draft consensus formulations that follow. We call this translational terminology our "D3 lingo" (or "Chalky Teeth Lingo") to emphasise how it works seamlessly from chatting with the public through to clinical and scientific discourse. This unique language – which is both "science-friendly" and "friendly science" – will necessarily evolve with growth in understanding and D3G's global reach. So please let us know what you think as we take this important terminological journey together (contact us).
IS TERMINOLOGY IMPORTANT?
If you're wondering whether terminology is of any real importance for practitioners, we say "yes!" in a word, and "more so than ever" in four. Of course we'd all love it if D3 problems went away, and past scientific wins have given good reason for further expectations in this regard (think tetracyclines and fluoride safety). Agreeing that practitioners will benefit from more science, it's a short step to appreciate that scientists will benefit reciprocally from having key terminology understood and used carefully by practitioners. Indeed, how else
will it be known we're all on the same page and stewing over the same problems? We think getting your head around our recommended terms need not be a hassle.
Indeed, realising that scientific intricacies can be a bit
overbearing at times, we've put our translational caps
on and worked hard to distill the key elements and
present them in an understandable and memorable way.
Besides intercommunication between practitioners and scientists, we also try to think "translationally" about others who will play a key role in fixing D3 problems – affected kids and families, public health professionals, and politicians too. Will one set of terms fit all these needs? We don't think so and for this reason have developed parallel vernaculars for kids and lay people, as you will see sprinkled throughout this website – a compilation appears in the glossary below. Hopefully you'll find it fun to participate in this community-focussed level of communication too.
DISTINGUISHING HYPOMIN AND HYPOPLASIA
What's the most common terminological mix-up in our field? – that's easy to answer, anecdotally at least. Failure to properly distinguish between "Hypomineralisation" and "Hypoplasia" appears to be a worldwide problem, for better or worse! Historically there has been little pressure on practitioners to get these terms right, to the extent that for many "hypoplasia" remains a catch-all for anything to do with missing enamel. But that situation is no longer tenable for two good reasons – the first of which is growing need for liaison between practitioners and scientists, as noted above. Secondly, and realistically of higher priority to most practitioners, the recent surge in clinical and scientific understanding of Molar Hypomin has led to a growing number of clinical imperatives. It follows that practitioners aspiring to best-care standards must respect Hypomin and Hypoplasia as clinically distinct entities.
So what are the key differences between Hypoplasia and Hypomin?Having realised why you need to understand the terminological differences between Hypomin and Hypoplasia, actually learning what they are is quite straightforward. Most simply, in our case Hypoplasia means a developmental deficiency in the thickness of enamel, whereas Hypomin refers to a deficit in its mineral content. The thickness deficit in Hypoplasia traces back to an early error during secretion of the developing enamel layer – and as a result, enamel Hypoplasias are always present before a tooth first enters the mouth. In contrast, the mineral deficit in Hypomin enamel happens later in development, after the enamel layer has been secreted – so Hypomin defects involve enamel of normal thickness, in unerupted teeth at least.
Why then the confusion?
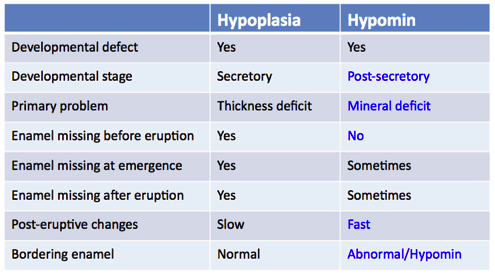 With such obvious differences between the two, how come there is so much confusion surrounding Hypomin and Hypoplasia? That too is quite simple to understand once you look at it from the clinical perspective, which mostly involves erupted teeth of course. Lacking the hardness and durability of normal enamel, Hypomin enamel is prone to degrade rapidly once exposed to the oral environment (e.g. masticatory forces, dietary acids). In severe cases, such "breakdown" may commence as soon as the tooth emerges through the gum ("eruptive breakdown") whereas in moderate cases the degradation may become obvious only after the tooth has erupted ("post-eruptive breakdown"). Because such degradation of Hypomin enamel doesn't happen before emergence, it is fundamentally incorrect to refer to it as Hypoplasia. Put another way, breakdown of Hypomin lesions represents an acquired deficit of enamel thickness, not a developmental one. Conversely, with Hypoplasia most enamel loss occurs before eruption, with any post-eruptive loss relatively minimal. Hence a key distinguishing feature of Hypomin is its relatively fast rate of change post-eruptively.
With such obvious differences between the two, how come there is so much confusion surrounding Hypomin and Hypoplasia? That too is quite simple to understand once you look at it from the clinical perspective, which mostly involves erupted teeth of course. Lacking the hardness and durability of normal enamel, Hypomin enamel is prone to degrade rapidly once exposed to the oral environment (e.g. masticatory forces, dietary acids). In severe cases, such "breakdown" may commence as soon as the tooth emerges through the gum ("eruptive breakdown") whereas in moderate cases the degradation may become obvious only after the tooth has erupted ("post-eruptive breakdown"). Because such degradation of Hypomin enamel doesn't happen before emergence, it is fundamentally incorrect to refer to it as Hypoplasia. Put another way, breakdown of Hypomin lesions represents an acquired deficit of enamel thickness, not a developmental one. Conversely, with Hypoplasia most enamel loss occurs before eruption, with any post-eruptive loss relatively minimal. Hence a key distinguishing feature of Hypomin is its relatively fast rate of change post-eruptively.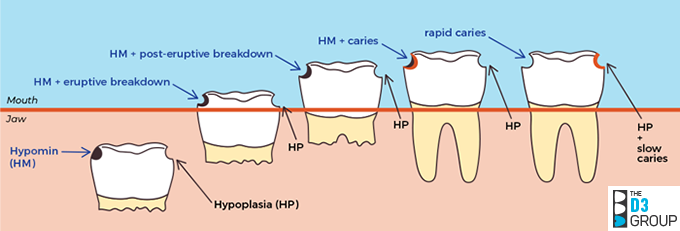
Any practical significance?
Finally, you might wonder whether this terminological distinction holds any practical significance for dental treatment? From what we understand so far, the answer appears to be a strong yes. Simply put, Hypomin starts out as a normal amount of abnormal enamel whereas Hypoplasia is the opposite – an abnormal amount of normal enamel. These clear-cut differences are likely to influence a variety of clinical decision points (e.g. etching/bonding, margins/restoratives, pain control), as noted in the following sections. So being able to discriminate between Hypoplasia and Hypomin properly can have a huge bearing on how you plan treatment of such teeth.
Understanding other basic D3 terms
Besides Hypomin and Hypoplasia, several other terms crop up regularly in our D3 world. A compilation of those terms used frequently in this website and D3G publications follows. We also include a colloquial adaptation of the international dental notation system, as often used in this part of the world to refer to tooth types collectively, plus a bit of practitioner slang that might also strike a chord with affected families and others.
|
TERM |
DRAFT DEFINITION |
|
D3s (enamel) |
Developmental Dental Defects (focussing here on enamel) |
|
Developmental defect |
The primary problem happened before eruption |
|
"Congenital", "birth defect" |
Lay terms for D3, okay if qualified to individual tooth (vs. baby) |
|
Genetic |
Developmental problem attributable to genetic anomaly |
|
Acquired |
Developmental problem not attributable to genetic anomaly |
|
Idiopathic |
Cause is unknown |
|
Lesion |
A patch of abnormal enamel |
|
Opacity |
A lesion lacking the translucence of normal enamel |
|
Discoloured |
A lesion with different colour from normal enamel |
|
Missing enamel |
A helpful term when uncertain about Hypomin vs. Hypoplasia etc |
|
Enamel Hypomin (HM) |
Hypomineralisation, a deficit in mineral content of enamel |
|
Demarcated opacity |
An opacity with sharply defined edges, typical of Molar Hypomin |
|
Diffuse opacity |
An opacity without sharply defined edges, typical of fluorosis |
|
Mottled enamel |
Scattered, diffuse opacities, typical of fluorosis |
|
Shiny surface |
Lesion reflects light similarly to normal enamel |
|
Frosted surface |
Lesion reflects light poorly relative to normal enamel |
|
Pitted surface |
Lesion with early degradation visible to eye |
|
Chalky enamel |
Discoloured & soft, can be cut by hand (moderate/severe Hypomin) |
|
Breakdown |
Degradation of Hypomin enamel, starting at surface |
|
Eruptive breakdown |
Breakdown of Hypomin enamel during emergence (severe Hypomin) |
|
Post-eruptive breakdown |
Breakdown of Hypomin enamel after eruption (moderate Hypomin) |
|
Intact lesion |
A hypomin lesion with intact surface enamel |
|
Broken lesion |
A hypomin lesion that has undergone breakdown (but not caries) |
|
Sharp margins |
Sharp irregular border, consistent with degradative fracture |
|
Enamel Hypoplasia (HP) |
A pre-eruptive (developmental) deficit in enamel thickness |
|
Rounded margins |
Rounded edge of normal enamel at border of hypoplastic lesion |
|
Regular outline |
A geometrically smooth lesion outline (e.g. groove, circular pit) |
|
Multi-tooth Notation |
Adapted from FDI World Dental Federation Notation, ISO 3950 |
|
6s, 7s & 8s |
First, second & third permanent molars |
|
1s & 2s |
First & second permanent incisors |
|
3s, 4s & 5s |
Canines, first & second permanent premolars |
|
Ds & Es |
First & second primary molars (from Palmer notation) |
|
Practitioner Slang |
Ex D3G members, and with a view to better consistency! |
|
Dodgy 6s |
"Potentially bad" Molar Hypomin but not necessarily a lost cause |
|
Manky molars |
Severe Molar Hypomin, connotes "maimed" & "poor hygiene" |
|
Bombed 6s |
Severe Molar Hypomin with carious involvement (i.e. cratered) |
|
Totally Bombed |
A lost cause, warranting "expedited tooth loss" |
|
Rotten |
Advanced caries in teeth unaffected by Hypomin |
Glossary for the translational vernacular used on this website
Aiming to have effective translational interactions across the sector (i.e. from scientists through to the public), we are trialling a multilevel vernacular for a variety of key D3 terms as follows.
|
CHILD |
LAYPERSON |
PRACTITIONER |
SCIENTIST |
|
Molar Hypomin |
|
|
|
|
Chalky Molars or Molar Hypomin |
Chalky Molars or Molar Hypomin |
Molar Hypomin or Hypomineralisation |
6s with Enamel Hypomineralisation |
|
6-year/12-year molar (adult molars) |
6-year/12-year molar (adult molars) |
First/second permanent molar | 6/7 |
| 1-year/2-year molar (baby molars) |
1-year/2-year molar (baby molars) |
First/second primary molar | D/E |
|
Wonky Tooth |
Hypomin tooth |
Hypomin tooth |
Enamel Hypomin (6) |
|
Wee Bit Wonky |
Minor defect |
Mild/intact |
Intact surface |
|
Fairly Wonky |
Moderate defect |
Moderate/frosted |
Frosted surface |
|
Really Wonky |
Severe defect |
Severe/broken |
Broken surface |
|
Bruise |
Mild patch |
Intact/mild lesion |
Intact lesion |
|
Chalky or Crumbly |
Chalky enamel or soft Hypomin enamel |
Early breakdown |
Surface pitting |
|
Pothole |
Hypomin hole/crater |
Advanced breakdown |
Broken lesion |
|
|
|
|
|
|
Caries |
|
|
|
|
Cavity |
Cavity/decay |
Carious lesion |
Carious lesion |
|
(rotten) passive use only? |
Decayed (rotten) |
Advanced caries |
Advanced caries |
|
|
|
|
|
|
Plaque |
|
|
|
|
Plaque Bugs |
Bacteria |
Oral bacteria |
Bacteria |
|
Plaque Cities |
Dental plaque |
Plaque, biofilm |
Plaque, biofilm |
|
|
|
|
|
|
Dental treatment |
|
|
|
|
Shiny Hat |
Metal crown |
Stainless steel crown |
Dental crown |
|
Wiggle out |
Remove/extract |
Extract |
Extract |
|
|
|
|
|
|
Dental Science |
|
|
|
|
Tooth Bricks |
Enamel rods |
Enamel rods/prisms |
Enamel prisms |
|
Tooth Mini-Bricks |
Mineral crystals |
Enamel crystallites |
Enamel crystallites |
|
Missing Bricks |
Soft, porous |
Porous/Hypomin |
Porous/Hypomin |

