D3G SPECIALISTS GUIDE FOR D3 TERMINOLOGY
Specialist Stuff
Building on the Basic Guidelines, here we consider additional terms and aim to define underlying "shades-of-grey" questions, as may be asked by experienced GPs and paediatric dental specialists. It should be realised that, as science brings us new information, some aspects will require revision. For instance, it was only in 2010 that Molar Hypomin was first characterised as a hypocalcification-type defect, bringing several implications for practitioners and researchers alike (see below).
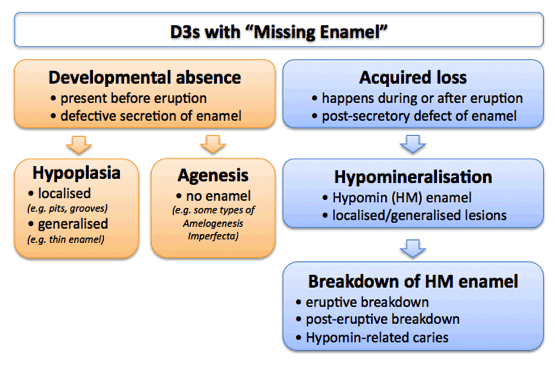
Accounting for Missing Enamel
Many reasons exist for missing enamel, including developmental abnormalities and traumatic loss. And in fact, "Missing Enamel" might be the best term to use in many cases, should a more-definitive diagnosis be lacking – it certainly is a much better catch-all than the "hypoplasia" misnomer. A draft depiction of the main developmental reasons for missing enamel, emphasising the distinction between Hypomin and Hypoplasia, follows.
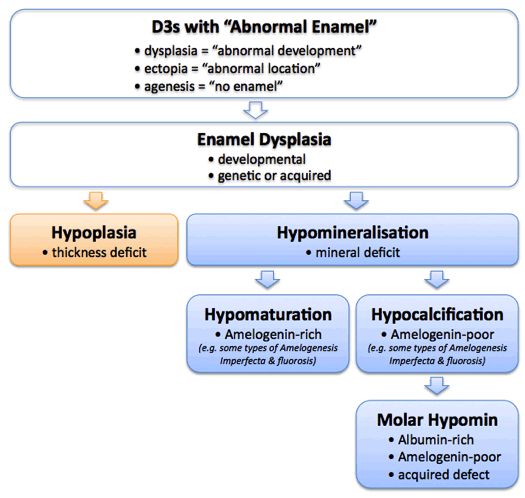
Categorising Molar Hypomin
Recent protein-profiling (proteomics) studies have enabled Molar Hypomin to be categorised as a new type of hypocalcification defect. Specifically, intact Hypomin lesions were found to have a low content of the intrinsic enamel protein Amelogenin, and a high content of the extrinsic protein Albumin. More than a terminological advance, these findings hold potential significance for the diagnosis, treatment and prevention of Molar Hypomin. A draft schematic relating this information to other categories of enamel malformation, and some links to associated literature, follows
Key literature
- Clinical classification of AI into three main subtypes – Witkop 1988
- Biochemical parameters for AI subtypes – Wright 1997, Takagi 1998
- Biochemical parameters for dental fluorosis – Wright 1996
- Biochemical parameters for Molar Hypomin – Mangum 2010, Williams 2020, Perez 2020
FAQ's
A. "Kids' Speak"
Q A1: I'm unfamiliar with terms such as Wee Bit Wonky – is there something better?
- is there a set of terms that better deals with grading of malformed teeth?
- is this child-friendly, distinctively memorable and fun at family level?
- as an Ozzie-Enzed network, should D3G be a wee bit proud to share our local lingo?
Q A2: Should we talk down to kids or instead teach them adult terms early?
- good question – and should this also apply to childhood myths (e.g. Tooth Fairy)?
- might a kids' vernacular be useful to head them down a structured-learning path?
Q A3: Is the "dental birth defect" analogy consistent with medical terminology?
- is there a better way of explaining "developmental dental defect" in simple terms?
- is "congenital/birth defect" wrong if qualified to the "birth" (eruption) of a tooth?
- note: medically, congenital defects exist at birth but are not necessarily apparent then
B. Hypomin vs Hypoplasia
Q B1: Should Hypomin be a first-pick term based on incidence?
- note: most studies report Hypomin >> Hypoplasia nowadays (e.g. 25-fold higher)
- but is "missing enamel" a safer term in uncertain situations?
Q B2: It's so hard to tell them apart clinically – why care about the terms?
- note: see this explanation please
- remember: correct terminology and diagnostic challenges are two different things
Q B3: Does it have to be an either/or decision?
- might an individual lesion have both Hypomin and Hypoplastic components?
- if so, which defect should take precedence – terminologically & treatment-wise?
C. Hypomineralisation
Q C1: What are the clinical features of Hypocalcification & Hypomaturation?
- note: Witkop described Hypomaturation-AI as rather soft & prone to chipping
- Hypocalcification-AI was distinguished as softer, friable/crumbly & prone to loss
- this accords with Hypomin 6s being dubbed "Cheese Molars" (also more recently)
- biochemical discriminators now exist but clinical diagnostics aren't available yet

